2Department of Cardiology, İzmir Katip Çelebi University Atatürk Training and Research Hospital, İzmir, Türkiye
3Department of Cardiology, Hitit University Erol Olçok Training and Research Hospital, Çorum, Türkiye
4Department of Cardiology, Ankara Etlik City Hospital, Ankara, Türkiye
5Department of Cardiology, Yozgat City Hospital, Yozgat, Türkiye
Abstract
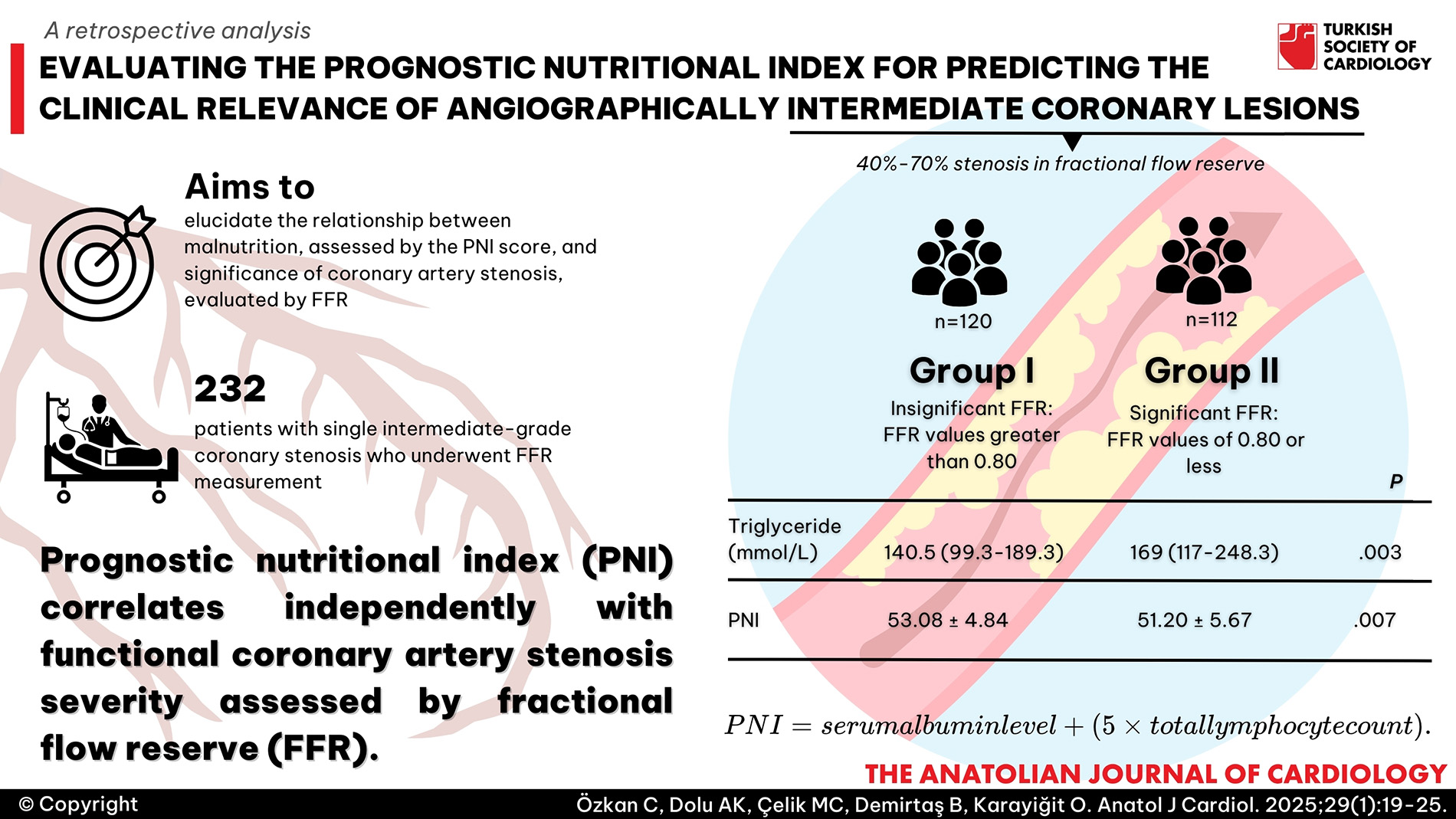
Background: Coronary artery disease (CAD) is a widespread health issue globally, linked to significant morbidity and mortality. While oxidative stress, dysregulated lipid metabolism, and unhealthy lifestyle choices contribute to CAD, recent research highlights the role of immune responses and inflammation. Malnutrition, a modifiable risk factor, notably impacts CAD prognosis. The prognostic nutritional index (PNI), derived from serum albumin and lymphocyte count, predicts outcomes in various diseases. This study aims to elucidate the relationship between malnutrition, as assessed by the PNI score, and the functional significance of coronary artery stenosis, evaluated by fractional flow reserve (FFR) measurements.
Methods: A retrospective analysis involved 232 patients with single intermediate-grade coronary stenosis who underwent FFR measurement between January 2022 and January 2024. Prognostic nutritional index values were calculated from serum albumin and lymphocyte counts. Patients were divided into 2 groups based on FFR values.
Results: Patients with hemodynamically significant coronary stenosis (FFR ≤ 0.80) exhibited higher inflammatory markers and triglycerides, while those with FFR > 0.80 showed elevated albumin and PNI levels. Triglycerides and PNI emerged as independent predictors of significant coronary stenosis.
Conclusions: This study demonstrates that PNI is independently associated with the functional significance of coronary artery stenosis as determined by FFR. Since lymphocytes, total protein and albumin values, which are readily available from routine blood tests, form the basis for PNI, this index can be easily used in clinical settings to predict hemodynamically significant coronary artery stenosis. However, the results of this study should be further expanded and validated through studies involving larger samples and prospective designs.
Graphical Abstract
Highlights
- Prognostic nutritional index (PNI) correlates independently with functional coronary artery stenosis severity assessed by fractional flow reserve (FFR).
- Elevated triglycerides and lower PNI values are predictive markers of hemodynamically significant coronary lesions.
- Prognostic nutritional index, derived from routine blood tests, offers a cost-effective tool for risk stratification in patients with intermediate coronary artery disease.
- Neutrophil levels and hypoalbuminemia are associated with the severity of coronary artery lesions assessed by FFR.
- Integrating PNI assessment into clinical practice could enhance prognostic evaluation and guide therapeutic strategies effectively.
Introduction
Coronary artery disease (CAD) is a prevalent disorder impacting millions globally, constituting 32.7% of all heart diseases and 1.7% of the total disease burden.1 It stands as a leading cause of both morbidity and mortality, imposing substantial medical and economic strains on society.2 Primarily, CAD onset is linked to oxidative stress, dysregulated lipid metabolism, and unhealthy lifestyle choices predisposing to thrombosis. However, contemporary research underscores the contribution of immune responses and inflammatory processes to CAD progression.3,
Malnutrition is a growing global concern and is recognized as a modifiable risk factor for various diseases. Its detrimental impact extends to the prognosis for individuals with acute coronary syndrome (ACS).5 Research indicates that over 40% of patients with heart failure suffer from malnutrition, and its presence serves as an independent predictor of mortality.6 Furthermore, a study revealed that more than 50% of CAD patients exhibit varying degrees of malnutrition, a factor predictive of adverse cardiac events.7
Albumin, a plasma protein crucial for maintaining plasma oncotic pressure, serves as a reliable indicator of nutritional status. Moreover, it possesses anti-inflammatory and antioxidative properties, including the binding of various toxins and scavenging free radicals. Lymphocytes, constituents of the white blood cell population, are pivotal during inflammatory processes.8 Prognostic nutritional index, easily calculable, offers insights into both nutritional and immunological statuses. Derived from serum albumin concentration and total lymphocyte count, it has been commonly utilized to anticipate complication risks post-gastrointestinal surgeries.9 Recent evidence highlights the prognostic significance of PNI following coronary artery bypass graft procedures, correlating with mortality and adverse events.10 Notably, in a local study involving patients with unprotected left main coronary artery undergoing percutaneous coronary intervention (PCI), malnourished individuals exhibited higher rates of all-cause mortality and stroke compared to their well-nourished counterparts, findings reflected in their PNI.11
Prognostic nutritional index is a biomarker of inflammation beyond nutritional status.12 Inflammation is recognized as an important risk factor for CAD.13 Different inflammatory markers have been used to predict hemodynamically severe lesions.14 However, there is insufficient data on whether PNI can predict hemodynamically significant lesions. A study by Zhang et al15 reported that malnutrition as assessed by PNI was independently predictive of mortality and major adverse cardiovascular events (MACEs) in CAD patients. In another study, nutritional status assessed by PNI was significantly and strongly associated with adverse cardiac events in patients after elective PCI and was identified as an independent predictor of long-term cardiovascular outcomes in patients with stable CAD after elective PCI.16
Intermediate coronary artery stenosis is a common finding in routine coronary angiography.17 Identifying and managing these moderate coronary lesions may offer potential advantages but presents significant challenges due to heightened procedural and long-term risks.18
Nevertheless, it is imperative to mitigate the risk of future MACE associated with culprit intermediate lesions.19 Fractional flow reserve (FFR), representing the ratio of maximum myocardial blood flow in a diseased artery to the maximum myocardial blood flow under normal conditions,20 has been substantiated by numerous clinical trials to significantly enhance patient outcomes, particularly when utilized for guiding coronary revascularization. Consequently, strategies informed by FFR have garnered the most robust endorsement in the latest guidelines for PCI. The optimization of this advantage necessitates scrupulous and standardized protocols governing the acquisition, documentation, storage, and transmission of FFR measurements within the realm of clinical investigations.21
Fractional flow reserve is the gold standard method used to assess whether lesions are hemodynamically significant. However, its disadvantages include an invasive procedure, possible complications, and increased cost. The PNI serves as a practical, applicable, and prognostic scoring system. In this context, our study aims to investigate the relationship between PNI-assessed malnutrition and FFR assessment in patients with moderate coronary artery stenosis. By investigating this association, our study aims to contribute to the understanding of the role of PNI as a practical, cost-effective biomarker for predicting hemodynamically significant coronary lesions and potentially provide new insights in CAD management.
Methods
This retrospective study was conducted over the period spanning from January 2022 to January 2024, encompassing a cohort of 232 consecutive patients. Among these, there were 63 female and 169 male individuals diagnosed with single intermediate-grade coronary stenosis (40%-70%, as determined by quantitative coronary analysis), all of whom underwent FFR measurement. The study population consisted of patients who had undergone coronary angiography due to stable angina pectoris. Exclusion criteria encompassed patients with ACS, moderate or severe valvular heart disease, significant arrhythmias, hemodynamic instability, a secondary lesion in the index coronary artery or presence of another coronary artery with ≥40% luminal narrowing, history of prior surgical or percutaneous coronary artery intervention, acute or chronic inflammatory or infectious conditions, anemia, chronic renal failure, or malignancy.
Data were collected from hospital records and files, including patients’ demographic, clinical, and angiographic information. Blood samples were obtained from venous sources within 24 hours of hospital admission and analyzed for lipid profile, serum creatinine levels, and complete blood count. Prognostic nutritional index was calculated using the formula: PNI = serum albumin level + (5 × total lymphocyte count).
Fractional flow reserve assessments were conducted on intermediate-grade lesions exhibiting a stenosis rate ranging between 40% and 70%, as determined at the discretion of cardiologists. Fractional flow reserve records were also obtained from the hospital’s registration system.
Fractional flow reserve values of 0.80 or less were considered indicative of hemodynamic significance. Patients were categorized into 2 groups: group I, with FFR values greater than 0.80, and group II, with FFR values of 0.80 or less.
Artificial Intelligence Statement
Artificial Intelligence-supported technologies were not used in the production of this submitted work.
Statistical Analysis
The necessary statistical analyses were performed using SPSS software version 20.0 for Windows (SPSS Inc., Chicago, IL, USA), and the distribution shapes of variables were analyzed using the Kolmogorov–Smirnov test. While categorical determinants were given as percentages and numbers, continuous variables were presented as mean ± standard deviation or median with interquartile range, depending on the distribution model of the variables. The Mann–Whitney
Results
Based on the presence of significant functional coronary stenosis, the study cohort was divided into 2 groups: group I comprised 120 patients (males: 84 (70%); mean age: 59 ± 9.69 years) without significant stenosis, while group II included 112 patients (males: 85 (75.9%); mean age: 57.6 ± 9.18 years) with significant stenosis.
Regarding laboratory parameters, group II demonstrated higher levels of white blood cells [9.25 (7.62-11.1) vs. 7.93 (6.83-9.82) × 103/µL,
Parameters identified as significant in the univariate logistic regression analysis were subsequently included in the multivariate logistic regression analysis to determine the predictors of hemodynamically significant coronary artery stenosis. TG (OR: 1.005, 95% CI: 1.002-1.008;
Receiver operating characteristic analysis revealed that a threshold value of 51.9 exhibited a sensitivity of 65.2% and a specificity of 64.2% in predicting hemodynamically significant coronary artery stenosis (AUC: 0.637, 95% CI: 0.564-0.710,
Discussion
In this study, PNI levels were independently associated with functionally significant coronary artery lesions evaluated by FFR measurement. Additionally, triglycerides remained one of the independent determinants of functional significance in the multivariable analysis. The concept of FFR has been developed as an index of the functional severity of coronary artery stenoses determined invasively.22 It represents the ratio of hyperemic myocardial blood flow in the stenotic region to hyperemic myocardial blood flow in the same region without narrowing.23 It is used when the severity of stenoses seen by coronary angiography cannot be clearly assessed qualitatively.24 Fractional flow reserve-guided PCI improves patient outcomes, reduces stent implantations, and lowers costs.25 Studies have found FFR to be superior to angiography when used to guide revascularization strategies and have shown that routine FFR measurement in patients with multivessel coronary artery disease reduces the rate of major adverse cardiac events.26,
The PNI emerges as an indicator of poor prognosis in individuals with cardiovascular disease.28 Initially utilized to monitor the nutritional status of postoperative patients, over time, PNI has been employed to predict outcomes in malignant tumors and coronary artery disease, with it being thought to reflect the systemic inflammatory state to a certain extent.29 Coronary artery disease develops on an atherosclerotic background, which involves lipid metabolism and specific inflammatory cytokines and processes.30 Therefore, inflammation is considered one of the most significant factors in the development of atherosclerosis.31 Furthermore, studies have reported an association between low PNI values and increased risk of MACE and cerebrovascular events.32 In a cohort study examining the relationship between diabetes, PNI, and the prognosis of coronary artery disease, Li et al33 demonstrated that patients with low PNI levels had a higher risk of all-cause mortality. Additionally, Ling et al34 showed in their study that PNI was an independent risk factor for all-cause mortality in patients who underwent PCI following acute myocardial infarction. In another study, it was found that low PNI values increased in-stent restenosis by activating inflammatory processes.35 Furthermore, a meta-analysis revealed that in patients with heart failure, PNI was identified as an independent predictor of all-cause mortality and/or readmission to the hospital.36 A study by Tolunay et al37 found that PNI was significantly associated with the Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery (SYNTAX) score, and PNI was associated with cardiovascular mortality and rehospitalization within 6 months of ACS diagnosis. In another study supporting our study, the severity of coronary lesions was found to be closely associated with PNI.38 In a study by Güzel et al11 examining long-term outcomes after left main coronary artery revascularization, a statistically significant relationship was found between PNI values and SYNTAX score. Another study investigated the relationship between nutritional status and prognosis in ST-elevation myocardial infarction (STEMI) patients and the main finding was that a controlling nutritional status score of ≥5 predicted an increased risk of MACE in STEMI patients at long-term follow-up. It has been suggested that scores used to estimate the degree of malnutrition may be more effective than parameters used alone, such as body mass index or serum albumin levels.39 All these studies show a correlation between the degree of coronary artery disease and PNI. In our study, FFR measurement was used to determine the functional significance of coronary lesions and their relationship with PNI levels. We found that patients with hemodynamically significant lesions, as assessed by FFR (FFR ≤ 0.80), had significantly lower PNI levels. In another respect, our study also shows that hemodynamically significant stenoses, as measured by FFR, are statistically significantly associated with PNI.
When examining the basal characteristic features of patients in the study, it was observed that in the group with hemodynamically significant FFR results, statistically significant hypoalbuminemia and elevated neutrophil counts were detected. Neutrophils significantly influence the onset and progression of notable atherosclerotic lesions.40 Therefore, high neutrophil levels may be associated with the hemodynamically significant FFR group. Acute-phase reactants are proteins that indirectly measure the inflammatory state. Albumin is one of the most well-known acute-phase reactants.41 Serum albumin levels serve as reliable predictors of cardiovascular diseases.42 Albumin has been associated with coronary artery disease through the response mechanism to inflammation. Numerous studies have reported the relationship between low serum albumin levels and increased risks of cardiovascular disease and heart failure. It has been suggested that serum albumin levels are inversely proportional to the incidence of ischemic heart disease. Low serum albumin levels are associated with platelet aggregation, impaired endothelial function, and thrombocyte-derived luminal narrowing in coronary arteries.43
In our study, we also observed that TG levels were significantly higher in the group with significant FFR results. Previous studies support the critical role of alterations in specific lipid or lipoprotein levels in the development of atherosclerosis. The importance of local vascular wall and systemic inflammation in the development of atherosclerosis has been clearly demonstrated. While dyslipidemia was previously considered predominant in the development of atherosclerosis, it is now accepted that inflammation and dyslipidemia are integrated.44 Elevated TG levels lead to the formation of TG-rich lipoproteins enriched with apolipoprotein C-III, which affect signaling pathways influencing nuclear factor kappa B and contribute to inflammation, leading to the development of fatty streaks and advanced atherosclerosis. Moreover, it has been shown that the cholesterol content in TG-rich lipoproteins predicts CAD risk better than low-density lipoprotein-cholesterol.45 High TG levels have been identified as an independent risk factor for the development of coronary artery disease and acute cardiovascular events.46
Our study underscores the value of the PNI as a tool to assess the functional significance of coronary lesions. Our research showing an independent association between low PNI levels and hemodynamically significant coronary stenosis highlights the potential role of PNI in improving risk stratification and guiding management strategies for CAD. This approach may improve patient outcomes by identifying those at higher risk for adverse cardiovascular events, thereby enabling more targeted interventions.
Study Limitations
This study has several limitations. Firstly, it is characterized by a retrospective design with a limited number of patients. Secondly, many other important inflammatory markers were not included in this study. Lastly, our analyses are based on a single PNI value; thus, we did not track changes over time and variations in PNI.
Conclusion
In conclusion, this study demonstrates that PNI is independently associated with the functional significance of coronary artery stenosis as determined by FFR. Given the accessibility and low cost of PNI derived from routine blood tests such as serum albumin and total lymphocyte count, it offers a practical and effective tool to predict significant coronary artery stenosis in clinical practice. Integrating PNI assessment into clinical practice may aid in the management of CAD patients with intermediate coronary lesions. Future research should further investigate the utility of PNI in various CAD contexts and its potential to complement existing diagnostic methods.
Footnotes
References
- Bauersachs R, Zeymer U, Brière J-B, Marre C, Bowrin K, Huelsebeck M. Burden of coronary artery disease and peripheral artery disease: a literature review. Cardiovasc Ther. 2019;2019():8295054-. https://doi.org/10.1155/2019/8295054
- Hay SI, Abajobir AA, Abate KH. Global, regional, and national disability-adjusted life-years (DALYs) for 333 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1260-1344. https://doi.org/10.1016/S0140-6736(17)32130-X
- Fox KA, Metra M, Morais J, Atar D. The myth of ‘stable’coronary artery disease. Nat Rev Cardiol. 2020;17(1):9-21. https://doi.org/10.1038/s41569-019-0233-y
- Malakar AK, Choudhury D, Halder B, Paul P, Uddin A, Chakraborty S. A review on coronary artery disease, its risk factors, and therapeutics. J Cell Physiol. 2019;234(10):16812-16823. https://doi.org/10.1002/jcp.28350
- Raposeiras Roubín S, Abu Assi E, Cespón Fernandez M. Prevalence and prognostic significance of malnutrition in patients with acute coronary syndrome. J Am Coll Cardiol. 2020;76(7):828-840. https://doi.org/10.1016/j.jacc.2020.06.058
- Hirose S, Matsue Y, Kamiya K. Prevalence and prognostic implications of malnutrition as defined by GLIM criteria in elderly patients with heart failure. Clin Nutr. 2021;40(6):4334-4340. https://doi.org/10.1016/j.clnu.2021.01.014
- Wang H, Liu F, Ma H. Associations between depression, nutrition, and outcomes among individuals with coronary artery disease. Nutrition. 2021;86():111157-. https://doi.org/10.1016/j.nut.2021.111157
- Dolapoglu A, Avci E, Kiris T, Bugra O. The predictive value of the prognostic nutritional index for postoperative acute kidney injury in patients undergoing on-pump coronary bypass surgery. J Cardiothorac Surg. 2019;14(1):74-. https://doi.org/10.1186/s13019-019-0898-7
- Kono T, Sakamoto K, Shinden S, Ogawa K. Pre-therapeutic nutritional assessment for predicting severe adverse events in patients with head and neck cancer treated by radiotherapy. Clin Nutr. 2017;36(6):1681-1685. https://doi.org/10.1016/j.clnu.2016.10.021
- Keskin M, İpek G, Aldağ M. Effect of nutritional status on mortality in patients undergoing coronary artery bypass grafting. Nutrition. 2018;48():82-86. https://doi.org/10.1016/j.nut.2017.10.024
- Güzel T, Avcı E, Kırış T. Effect of the prognostic nutrition index on long-term outcomes in unprotected left main coronary artery revascularization. Kardiologiia. 2023;63(11):73-79. https://doi.org/10.18087/cardio.2023.11.n2367
- Chen MY, Wen JX, Lu MT. Association between prognostic nutritional index and prognosis in patients with heart failure: a meta-analysis. Front Cardiovasc Med. 2022;9():918566-. https://doi.org/10.3389/fcvm.2022.918566
- Sun M, Zhu S, Wang Y. Effect of inflammation on association between cancer and coronary artery disease. BMC Cardiovasc Disord. 2024;24(1):72-. https://doi.org/10.1186/s12872-023-03613-0
- Erdoğan M, Erdöl MA, Öztürk S, Durmaz T. Systemic immune-inflammation index is a novel marker to predict functionally significant coronary artery stenosis. Biomark Med. 2020;14(16):1553-1561. https://doi.org/10.2217/bmm-2020-0274
- Zhang S, Wang H, Chen S. Prognostic nutritional index and prognosis of patients with coronary artery disease: a systematic review and meta-analysis. Front Nutr. 2023;10():1114053-. https://doi.org/10.3389/fnut.2023.1114053
- Wada H, Dohi T, Miyauchi K. Relationship between the prognostic nutritional index and long-term clinical outcomes in patients with stable coronary artery disease. J Cardiol. 2018;72(2):155-161. https://doi.org/10.1016/j.jjcc.2018.01.012
- Hahn J-Y, Choi S-H, Jeong J-O. Conservative versus aggressive treatment strategy with angiographic guidance alone in patients with intermediate coronary lesions: the SMART-CASE randomized, non-inferiority trial. Int J Cardiol. 2017;240():114-119. https://doi.org/10.1016/j.ijcard.2017.03.075
- D’Ascenzo F, Bollati M, Clementi F. Incidence and predictors of coronary stent thrombosis: evidence from an international collaborative meta-analysis including 30 studies, 221,066 patients, and 4276 thromboses. Int J Cardiol. 2013;167(2):575-584. https://doi.org/10.1016/j.ijcard.2012.01.080
- Moses JW, Stone GW, Nikolsky E. Drug-eluting stents in the treatment of intermediate lesions: pooled analysis from four randomized trials. J Am Coll Cardiol. 2006;47(11):2164-2171. https://doi.org/10.1016/j.jacc.2006.01.068
- De Bruyne B, Sarma J. Fractional flow reserve: a review: invasive imaging. Heart. 2008;94(7):949-959. https://doi.org/10.1136/hrt.2007.122838
- Toth GG, Johnson NP, Jeremias A. Standardization of fractional flow reserve measurements. J Am Coll Cardiol. 2016;68(7):742-753. https://doi.org/10.1016/j.jacc.2016.05.067
- Pijls NH, de Bruyne B, Peels K. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med. 1996;334(26):1703-1708. https://doi.org/10.1056/NEJM199606273342604
- De Bruyne B, Pijls N, Bartunek J. Fractional flow reserve in patients with prior myocardial infarction. Circulation. 2001;104(2):157-162.
- Tobis J, Azarbal B, Slavin L. Assessment of intermediate severity coronary lesions in the catheterization laboratory. J Am Coll Cardiol. 2007;49(8):839-848. https://doi.org/10.1016/j.jacc.2006.10.055
- Morris PD, van de Vosse FN, Lawford PV, Hose DR, Gunn JP. “Virtual”(computed) fractional flow reserve: current challenges and limitations. JACC Cardiovasc Intv. 2015;8(8):1009-1017.
- Nogic J, Prosser H, O’Brien J. The assessment of intermediate coronary lesions using intracoronary imaging. Cardiovasc Diagn Ther. 2020;10(5):1445-1460. https://doi.org/10.21037/cdt-20-226
- Tonino PA, De Bruyne B, Pijls NH. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360(3):213-224. https://doi.org/10.1056/NEJMoa0807611
- Tonet E, Campana R, Caglioni S. Tools for the assessment of the malnutrition status and possible interventions in elderly with cardiovascular diseases. J Clin Med. 2021;10(7):1508-. https://doi.org/10.3390/jcm10071508
- Zhong X, Xie Y, Wang H, Chen G, Yang T, Xie J. Values of prognostic nutritional index for predicting Kawasaki disease: a systematic review and meta-analysis. Front Nutr. 2024;11():1305775-. https://doi.org/10.3389/fnut.2024.1305775
- Christodoulidis G, Vittorio TJ, Fudim M, Lerakis S, Kosmas CE. Inflammation in coronary artery disease. Cardiol Rev. 2014;22(6):279-288. https://doi.org/10.1097/CRD.0000000000000006
- Inoue T, Croce K, Morooka T, Sakuma M, Node K, Simon DI. Vascular inflammation and repair: implications for re-endothelialization, restenosis, and stent thrombosis. JACC Cardiovasc Intv. 2011;4(10):1057-1066. https://doi.org/10.1016/j.jcin.2011.05.025
- Sun S, Wang Y, Pang S, Wu X. Combination of the glycated hemoglobin levels and prognostic nutritional index as a prognostic marker in patients with acute coronary syndrome and type 2 diabetes mellitus. Lipids Health Dis. 2024;23(1):12-. https://doi.org/10.1186/s12944-023-01992-z
- Li T, Yuan D, Wang P. Association of prognostic nutritional index level and diabetes status with the prognosis of coronary artery disease: a cohort study. Diabetol Metab Syndr. 2023;15(1):58-.
- Ling X, Lin C, Liu J. Prognostic value of the prognostic nutritional index for patients with acute myocardial infarction undergoing percutaneous coronary intervention with variable glucose metabolism statuses: a retrospective cohort study. Diabetol Metab Syndr. 2023;15(1):207-. https://doi.org/10.1186/s13098-023-01160-4
- Balun A, Akgümüş A, Özbek K, Güven Çetin Z. Prognostic nutritional index as a novel predictor of in-stent restenosis: a retrospective study. Medicina (Kaunas). 2023;59(4):663-. https://doi.org/10.3390/medicina59040663
- Zhang X, Su Y. Low Prognostic nutritional index predicts adverse outcomes in patients with heart failure: a systematic review and meta-analysis. Angiology. 2024;75(4):305-313. https://doi.org/10.1177/00033197231159680
- Tolunay H, Görmel S, Asil S. The role of nutritional indexes in predicting coronary artery disease severity in acute coronary syndrome. Gulhane Med J. 2021;63(2):147-152. https://doi.org/10.4274/gulhane.galenos.2021.62207
- Li T, Yuan D, Wang P. Association of prognostic nutritional index level and diabetes status with the prognosis of coronary artery disease: a cohort study. Diabetol Metab Syndr. 2023;15(1):58-. https://doi.org/10.1186/s13098-023-01019-8
- Zengin A, Karataş MB, Çanga Y. Prognostic performance of Controlling Nutritional Status score in patients with ST segment elevation myocardial infarction treated with primary percutaneous coronary intervention. Anatol J Cardiol. 2022;26(1):23-28. https://doi.org/10.5152/AnatolJCardiol.2021.190
- Döring Y, Soehnlein O, Weber C. Neutrophil extracellular traps in atherosclerosis and atherothrombosis. Circ Res. 2017;120(4):736-743. https://doi.org/10.1161/CIRCRESAHA.116.309692
- McFarland DC, Breitbart W, Miller AH, Nelson C. Depression and inflammation in patients with lung cancer: a comparative analysis of acute phase reactant inflammatory markers. Psychosomatics. 2020;61(5):527-537. https://doi.org/10.1016/j.psym.2020.03.005
- Arques S. Human serum albumin in cardiovascular diseases. Eur J Intern Med. 2018;52():8-12. https://doi.org/10.1016/j.ejim.2018.04.014
- Özkan C, Karayiğit O. Relationship between high sensitivity C-reactive protein to albumin ratio with infarct-related artery patency in patients with non-ST-segment elevation myocardial infarction. Angiology. 2024;75(7):682-688. https://doi.org/10.1177/00033197231176983
- Schwartz EA, Reaven PD. Lipolysis of triglyceride-rich lipoproteins, vascular inflammation, and atherosclerosis. Biochim Biophys Acta. 2012;1821(5):858-866. https://doi.org/10.1016/j.bbalip.2011.09.021
- Welty FK. How do elevated triglycerides and low HDL-cholesterol affect inflammation and atherothrombosis?. Curr Cardiol Rep. 2013;15(9):400-. https://doi.org/10.1007/s11886-013-0400-4
- Sarwar N, Danesh J, Eiriksdottir G. Triglycerides and the risk of coronary heart disease: 10 158 incident cases among 262 525 participants in 29 Western prospective studies. Circulation. 2007;115(4):450-458. https://doi.org/10.1161/CIRCULATIONAHA.106.637793


