2Department of Cardiology, Alanya Training and Research Hospital, Antalya, Türkiye
Abstract
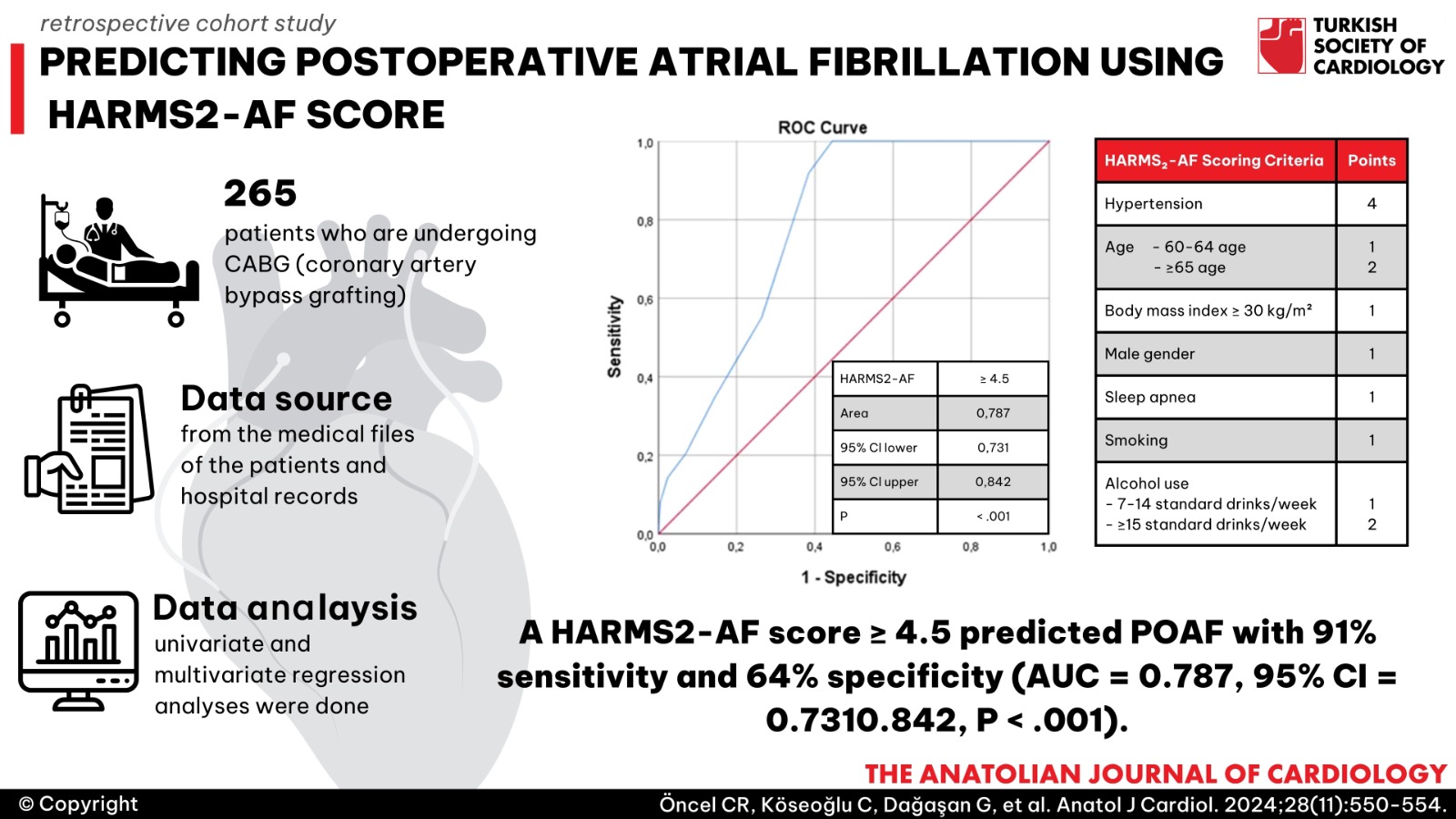
Background: Postoperative atrial fibrillation (POAF) remains a common complication after cardiac surgery. The ability to accurately identify patients at risk through previous risk scores is limited. This study aimed to evaluate the new HARMS2-AF risk score to predict POAF after coronary artery bypass grafting (CABG) surgery.
Methods: In this retrospective cohort study, we included 265 patients undergoing CABG surgery from 2022-2023. Data were obtained from the medical files of the patients and hospital records. Each patient was assigned a HARMS2-AF risk score. A univariate and multivariate regression analyses were done to analyze independent predictors of POAF.
Results: Of 265 patients, 49 had postoperative atrial fibrillation. HARMS2-AF score was significantly higher in patients with POAF. Age, sleep apnea, left atrial diameter (LAd), and HARMS2-AF score were independently associated with POAF. A HARMS2-AF score ≥ 4.5 predicted POAF with 91% sensitivity and 64% specificity (AUC = 0.787, 95% CI = 0.731-0.842, P < .001).
Conclusion: The HARMS2-AF score is a strong predictor of atrial fibrillation (AF) development after isolated CABG surgery. It can be used as a novel stratification tool to estimate AF after cardiac surgery.
Graphical Abstract
Highlights
- Postoperative atrial fibrillation (POAF) is associated with an increased mortality and morbidity, including a higher risk of ischemic stroke after coronary artery bypass surgery.
- HARMS-AF score is a new risk score that evaluates established and emerging lifestyle factors on incident AF risk.
- HARMS-AF score could be used to identify patients at the highest risk of developing POAF, thus avoiding nonselective arrhythmia prophylaxis as well as triggering aggressive risk factor management.
Introduction
Postoperative atrial fibrillation (POAF) is an important complication after coronary artery bypass graft (CABG) surgery, which occurs in nearly 30% of cases.1 It is associated with increased mortality and morbidity, including a higher risk of ischemic stroke.2
It has been demonstrated that patients with hypertension, diabetes mellitus, obesity, increased age, degenerative or rheumatic valvular heart disease, left atrial remodeling, and enlargement were under risk for development of POAF.3 Several studies have focused on identifying the demographic and clinical characteristics of POAF patients and related risk factors. Altered sympathetic activity with increased oxidative stress, as well as exaggerated inflammatory status during the postoperative period, is thought to be the underlying pathophysiological mechanisms.4
A simple, reproducible, and cost-effective scoring system needs to be developed to predict the probability of POAF because routine prophylactic antiarrhythmic treatment is associated with adverse clinical events and impaired surgical improvement. The HARMS2-AF score is a new risk score that evaluates established and emerging lifestyle factors on incident AF risk.5
In the present study, we aimed to evaluate the utility of the HARMS2-AF score in predicting the risk of developing POAF in CABG surgery patients to provide earlier prophylactic interventions to high-risk patients in the preoperative period.
Methods
This retrospective study evaluated a total of 310 patients who underwent isolated CABG surgery from September 2021-January 2024 at a university hospital. Data were obtained from the medical records of the patients. Patients with previous atrial fibrillation/flutter, acute coronary syndrome, renal failure, significant valvular heart disease, thyroid dysfunction, or heart failure (45 patients) were excluded from the study. The Local Ethics Committee approved the study protocol.
HARMS2-AF score refers to hypertension (4 points), age (60-64 years: 1 point; ≥65 years: 2 points), increased body mass index (BMI) (≥ 30 kg/m2: 1 point), gender (male sex: 2 points), sleep apnea (2 points), smoking (1 point), alcohol (7-14 standard drinks/week: 1 point; ≥15 standard drinks/week: 2 points) (
Surgical Technique
The patients underwent on-pump CABG surgery using a conventional technique. To summarize, after a median sternotomy, the ascending aorta was cannulated for the arterial line, and a single-stage venous cannula was inserted via the right atrial auricle. Aortic root venting and cold crystalloid cardioplegia were administered via the antegrade route. Cardiopulmonary bypass (CPB) with moderate systemic hypothermia (30-32°C) and hemodilution (Hct > 0.22) was the technique used. Antegrade cold crystalloid cardioplegia was administered sporadically to each subject. Peripheral and central anastomoses were created as a result of a single aortic blockage. The bypass conduits were either the saphenous veins, the internal mammary artery, or both.
Postoperative Follow-ups
We monitored the patients while they were in the hospital, keeping in mind that the risk of atrial fibrillation after surgery rises about 48 hours after the procedure. We analyzed ECG readings, in-hospital progress notes, nursing charts, discharge notes, and replies for cardiologist consultation, in addition to using postoperative diagnosis based on the International Classification of Diseases-10 categories. We also noted patients with postoperative atrial fibrillation who needed electrical cardioversion for rhythm or rate control, or who needed intravenous antiarrhythmic medication such as amiodarone, beta-blockers, propafenone, diltiazem, or verapamil.
Statistical Analysis
The normal distribution was evaluated using the Kolmogorov–Smirnov test. Categorical variables were identified using numbers and percentages, whereas continuous variables were expressed using mean ± SD. Continuous variables were compared using either a 1-way analysis of variance (ANOVA) or the Student’s
The forward elimination strategy using default values was used to identify prognostic factors. In the context of the Bonferroni multiple comparison test, statistical significance was determined by a
Results
Of the 310 patients who underwent CABG surgery during the study protocol, 265 patients were included in the analysis. The enrolled patients were classified into 2 groups according to the occurrence of postoperative AF or maintained sinus rhythm after coronary artery bypass surgery (POAF group vs. NPOAF group). Postoperative new-onset AF occurred in 49 (18.4%) patients. It was studied with a margin of error of 0.04 within a 96% confidence interval. The baseline demographic and clinical characteristics of the study subjects are shown in
When the demographic, clinical, and echocardiographic data of the groups are evaluated, the number of patients with hypertension (
The univariate logistic regression analysis showed that preoperative left ventricular ejection fraction (LVEF), left atrium diameter (LAd), aortic cross-clamp time, and HARMS2-AF scores were associated with postoperative AF. In the multivariate logistic regression analysis carried out after the formation of the model based on the parameters related to AF development, the relationship with HARMS2-AF score, LAd, and aortic cross-clamp time were observed to be prevalent (OR = 1.261, 95% CI = 1.174-1.554
As analyzed by the ROC curve, a HARMS2-AF score ≥ 4.5 predicted postoperative AF with 91% sensitivity and 64% specificity (AUC = 0.787, 95% CI = 0.731-0.842,
Discussion
The results of the present study showed that a higher HARMS2-AF score was significantly associated with an increased risk of developing postoperative atrial fibrillation. Previously, several risk factors, including advanced age, sex, diabetes mellitus, heart failure, and left atrial enlargement, were demonstrated independently in predicting POAF.6,
HARMS2-AF risk score is the first atrial fibrillation (AF) risk score which takes the relative contribution of lifestyle factors to AF development into consideration. The primary purpose of this AF score is to help physicians determine at-risk patients and potentially establish management of AF symptom burden, disease progression, as well as complications. This score includes 4 categorical (hypertension, male sex, sleep apnea, smoking) and 3 continuous (age, body mass index, alcohol consumption).10 Lu et al11 showed that regular smoking was associated with an increased risk of AF independent of the age at initiation or the number of cigarettes smoked per day. They also showed that heavy alcohol intake was linked to an increased risk of AF. Wang et al12 demonstrated that the prevalence of AF was significantly common in older patients with obstructive sleep apnea (OSA). The prevalence of AF was 9.5% and tended to further increase with OSA severity. In fact, multiple risk factors are common to OSA and AF. Obesity, advanced age, male gender, alcohol use, and smoking are important etiological components of OSA.13 In addition, a strong link between obesity and the risk of developing POAF has been demonstrated previously.14 Also concurrent with the literature, men develop postoperative atrial fibrillation at higher rates than do women.15
As POAF is associated with poor clinical outcomes, risk models are needed to guide POAF risk stratification in cardiac surgery patients. Existing clinical risk scores, such as EUROSCOREII, Society of Thoracic Surgeons, EUROSCORE, CHADS2, POAF score, HATCH, CHADS2VASC, and SYNTAX scores, offer at best moderate prediction for AF after cardiac surgery.16-
HARMS2-AF risk score could be a better model for risk stratification as it includes individual lifestyle risk factors to AF development that have previously been shown to be important. In our study, we revealed that age, left atrium diameter, sleep apnea, and HARMS2-AF score were significantly associated with AF after CABG. On the other hand, in the univariate logistic regression analysis, we found that although these risk factors are critical determinants of POAF, HARMS2-AF score was the optimal and accessible variable in predicting AF after CABG, as assessed by multivariate logistic regression analysis. Also in our study, the cutoff value for HARMS2-AF score was ≥ 4.5, indicating a sensitivity of 91% and specificity of 64%.
Several organizations have produced guidelines for prophylaxis against POAF.21-
Our study has several limitations. The major limitation is its retrospective design. Second, our study findings are limited to
Conclusion
In conclusion, identifying high-risk patients for POAF may prevent adverse cardiovascular events. Based on our study findings, the HARMS2-AF score is a strong predictor of atrial fibrillation development after isolated CABG. We believe that our study may inspire further studies using the HARMS2-AF scoring system to provide prophylactic atrial fibrillation therapies to high-risk patients preoperatively.
Footnotes
References
- Kashani RG, Sareh S, Genovese B. Predicting postoperative atrial fibrillation using CHA2DS2-VASc scores. J Surg Res. 2015;198(2):267-272. https://doi.org/10.1016/j.jss.2015.04.047
- LaPar DJ, Speir AM, Crosby IK. Postoperative atrial fibrillation significantly increases mortality, hospital readmission, and hospital costs. Ann Thorac Surg. 2014;98(2):527-533. https://doi.org/10.1016/j.athoracsur.2014.03.039
- Maesen B, Nijs J, Maessen J, Allessie M, Schotten U. Post-operative atrial fibrillation: a maze of mechanisms. Europace. 2012;14(2):159-174. https://doi.org/10.1093/europace/eur208
- Echahidi N, Pibarot P, O’Hara G, Mathieu P. Mechanisms, prevention, and treatment of atrial fibrillation after cardiac surgery. J Am Coll Cardiol. 2008;51(8):793-801. https://doi.org/10.1016/j.jacc.2007.10.043
- Segan L, Canovas R, Nanayakkara S. New-onset atrial fibrillation prediction: the HARMS2-AF risk score. Eur Heart J. 2023;44(36):3443-3452. https://doi.org/10.1093/eurheartj/ehad375
- Erdem K, Yazıcı M, Öztürk S, Avcı A, Güler Y, Erdem Hızal F. Usefulness of CHA2DS2-VASc scoring system in predicting atrial fibrillation after coronary artery bypass grafting. Turk Gogus Kalp Dama. 2016;24(1):27-33. https://doi.org/10.5606/tgkdc.dergisi.2016.11751
- Uysal D, Aksoy F, Ibrişim E. The validation of the ATRIA and CHA2DS2-Vasc scores in predicting atrial fibrillation after coronary artery bypass surgery. Braz J Cardiovasc Surg. 2020;35(5):619-625. https://doi.org/10.21470/1678-9741-2019-0274
- Villareal RP, Hariharan R, Liu BC. Postoperative atrial fibrillation and mortality after coronary artery bypass surgery. J Am Coll Cardiol. 2004;43(5):742-748. https://doi.org/10.1016/j.jacc.2003.11.023
- Mathew JP, Fontes ML, Tudor IC. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291(14):1720-1729. https://doi.org/10.1001/jama.291.14.1720
- Marcus GM. Translating HARMS2-AF into benefits for our atrial fibrillation patients and the general public: challenges and opportunities. Eur Heart J. 2023;44(36):3453-3455. https://doi.org/10.1093/eurheartj/ehad423
- Lu Y, Guo Y, Lin H, Wang Z, Zheng L. Genetically determined tobacco and alcohol use and risk of atrial fibrillation. BMC Med Genomics. 2021;14(1):73-. https://doi.org/10.1186/s12920-021-00915-0
- Wang H, Li J, Gao Y. Prevalence and factors associated with atrial fibrillation in older patients with obstructive sleep apnea. BMC Geriatr. 2022;22(1):204-. https://doi.org/10.1186/s12877-022-02791-4
- Sankaranarayanan R, Bansal A, Yanamaladoddi VR. Atrial fibrillation in obstructive sleep apnea patients: mechanisms, risk factors, and management strategies. Cureus. 2023;15(3):e36282-. https://doi.org/10.7759/cureus.36282
- Zacharias A, Schwann TA, Riordan CJ, Durham SJ, Shah AS, Habib RH. Obesity and risk of new-onset atrial fibrillation after cardiac surgery. Circulation. 2005;112(21):3247-3255. https://doi.org/10.1161/CIRCULATIONAHA.105.553743
- Westerman S, Wenger N. Gender differences in atrial fibrillation: a review of epidemiology, management, and outcomes. Curr Cardiol Rev. 2019;15(2):136-144. https://doi.org/10.2174/1573403X15666181205110624
- Pandey A, Okaj I, Ichhpuniani S. Risk scores for prediction of postoperative atrial fibrillation after cardiac surgery: a systematic review and meta-analysis. Am J Cardiol. 2023;209():232-240. https://doi.org/10.1016/j.amjcard.2023.08.161
- Patel N, Joglar JA. Postoperative atrial fibrillation after cardiac surgery and the challenges of predicting risk. Am J Cardiol. 2023;209():241-. https://doi.org/10.1016/j.amjcard.2023.09.043
- Chen YL, Zeng M, Liu Y. CHA2DS2-VASc score for identifying patients at high risk of postoperative atrial fibrillation after cardiac surgery: a meta-analysis. Ann Thorac Surg. 2020;109(4):1210-1216. https://doi.org/10.1016/j.athoracsur.2019.07.084
- Segar MW, Marzec A, Razavi M. Incidence, risk score performance, and in-hospital outcomes of postoperative atrial fibrillation after cardiac surgery. Tex Heart Inst J. 2023;50(5):e238221-. https://doi.org/10.14503/THIJ-23-8221
- Cameron MJ, Tran DTT, Abboud J, Newton EK, Rashidian H, Dupuis JY. Prospective external validation of three preoperative risk scores for prediction of new onset atrial fibrillation after cardiac surgery. Anesth Analg. 2018;126(1):33-38. https://doi.org/10.1213/ANE.0000000000002112
- Fuster V, Rydén LE, Cannom DS. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in partnership with the European Society of Cardiology and in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. J Am Coll Cardiol. 2011;57(11):e101-e198. https://doi.org/10.1016/j.jacc.2010.09.013
- Fernando HC, Jaklitsch MT, Walsh GL. The Society of Thoracic Surgeons practice guideline on the prophylaxis and management of atrial fibrillation associated with general thoracic surgery: executive summary. Ann Thorac Surg. 2011;92(3):1144-1152. https://doi.org/10.1016/j.athoracsur.2011.06.104
- Bradley D, Creswell LL, Hogue CW. Pharmacologic prophylaxis: American College of Chest Physicians guidelines for the prevention and management of postoperative atrial fibrillation after cardiac surgery. Chest. 2005;128(2 suppl):39S-47S. https://doi.org/10.1378/chest.128.2_suppl.39s
- Weber UK, Osswald S, Huber M. Selective versus non-selective antiarrhythmic approach for prevention of atrial fibrillation after coronary surgery: is there a need for pre-operative risk stratification? A prospective placebo- controlled study using low-dose sotalol. Eur Heart J. 1998;19(5):794-800. https://doi.org/10.1053/euhj.1997.0838
- Mariscalco G, Biancari F, Zanobini M. Bedside tool for predicting the risk of postoperative atrial fibrillation after cardiac surgery: the POAF score. J Am Heart Assoc. 2014;3(2):e000752-. https://doi.org/10.1161/JAHA.113.000752


