2Department of Cardiovascular Surgery, Faculty of Medicine, Mersin University, Mersin, Türkiye
Abstract
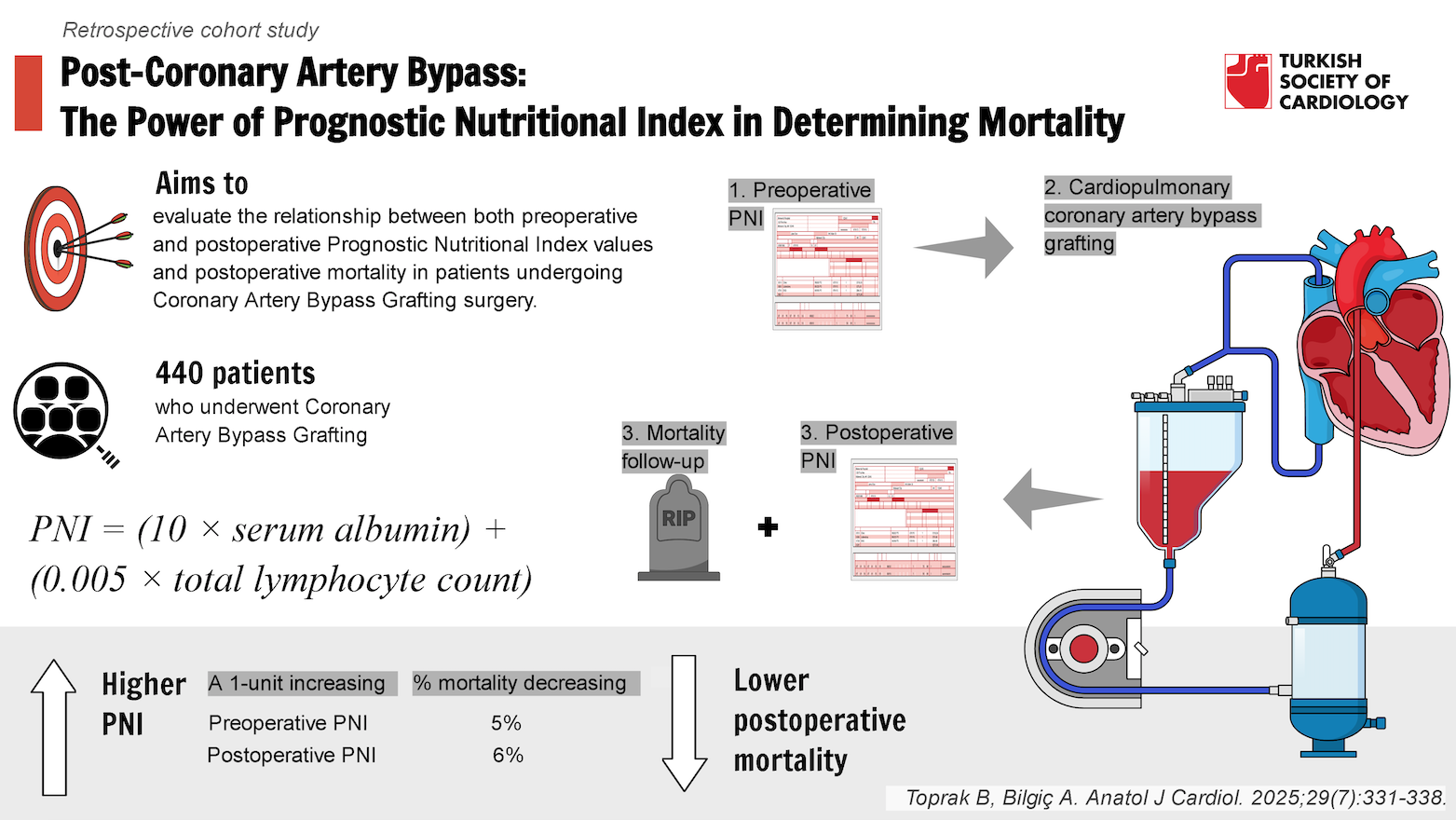
Background: The objective of this study was to evaluate the relationship between both preoperative and postoperative Prognostic Nutritional Index values and postoperative mortality in patients undergoing Coronary Artery Bypass Grafting surgery.
Methods: This retrospective cohort study included 440 patients who underwent Coronary Artery Bypass Grafting between March 2021 and April 2023. Preoperative and postoperative Prognostic Nutritional Index values were calculated based on serum albumin concentration and peripheral blood lymphocyte count. The primary outcome was mortality, with statistical analyses performed to assess the association between Prognostic Nutritional Index values (preoperative and postoperative) and mortality using univariate and multivariate methods.
Results: A significant correlation was found between low preoperative Prognostic Nutritional Index and increased postoperative mortality risk (P < .05). A 1-unit increase in preoperative Prognostic Nutritional Index was associated with a 5% reduction in mortality risk (Odds ratio [OR] = 0.95, P < .001, 95% CI: 0.96-0.98). Similarly, the postoperative Prognostic Nutritional Index was significantly associated with mortality, with a 1-unit increase in postoperative Prognostic Nutritional Index corresponding to a 6% reduction in mortality risk (OR = 0.94, P < .001, 95% CI: 0.92-0.96). Both preoperative and postoperative Prognostic Nutritional Index values independently predicted mortality risk, with postoperative Prognostic Nutritional Index showing a stronger association with mortality outcomes.
Conclusions: The study demonstrates that both preoperative and postoperative Prognostic Nutritional Index values are critical predictors of mortality risk in Coronary Artery Bypass Grafting patients. Early assessment of the Prognostic Nutritional Index, both preoperatively and postoperatively, could enhance risk stratification and improve patient outcomes through timely interventions.
Graphical Abstract
Highlights
- Both preoperative and postoperative prognostic nutritional index values are strong, independent predictors of mortality in coronary artery bypass grafting patients.
- A 1-unit increase in preoperative prognostic nutritional index reduces mortality risk by 2%, while a 1-unit increase in postoperative prognostic nutritional index reduces mortality risk by 4%.
- Postoperative prognostic nutritional index shows a stronger correlation with mortality outcomes compared to the preoperative prognostic nutritional index.
- Early evaluation of the prognostic nutritional index, both preoperatively and postoperatively, can significantly improve risk stratification and help optimize patient management.
- Postoperative reductions in the prognostic nutritional index highlight its critical role in predicting early mortality, stressing the importance of regular monitoring in the perioperative period.
Introduction
Coronary artery disease (CAD) is a significant health issue, causing over 4.5 million deaths annually in developing countries. It ranks as a leading cause of cardiovascular mortality worldwide.1 Studies have shown that Coronary Artery Bypass Grafting (CABG) surgery not only improves overall health-related quality of life but also significantly reduces mortality rates.2,
Despite advancements in technology and surgical techniques, efforts to reduce the high risk of mortality and morbidity in patients undergoing heart surgery have proven largely ineffective.9-
Prognostic nutritional index, which is calculated from serum albumin concentration and peripheral blood lymphocyte count, serves as a crucial indicator of nutritional status. Recent studies have highlighted the adverse effects of low PNI on surgical outcomes, particularly in hemodialysis-dependent patients undergoing cardiac surgery.20 Future research should also focus on assessing PNI in diverse populations, as variations in comorbidities may influence its predictive value. This study evaluates the predictive role of PNI findings on in-hospital mortality in patients undergoing CABG.
Methods
This retrospective, observational cohort study was conducted at Mersin University School of Medicine Education and Research Hospital, a single tertiary academic hospital serving the cardiovascular surgery department. The study included consecutive patients who underwent CABG between March 1, 2021, and April 30, 2023. To minimize selection bias, a propensity score matching (PSM) method was applied. Patients were matched based on age, sex, left ventricular ejection fraction (EF), and the presence of comorbidities such as diabetes mellitus (DM) and hypertension (HT).
Data Collection
A nested case-control design was used within the cohort to compare factors anticipated to be associated with mortality. An exposure odds ratio of 1.5 (considered the smallest clinically significant) was set, with a 25% width of the CI. The sample size for the study was determined to be 440 patients. The number of deceased patients was matched in a 1:4 ratio to the number of survivors.
Data on patients’ demographics, laboratory test results, procedure duration, left ventricular EF, and presence of multi-vessel disease were analyzed according to a predetermined protocol. Venous blood samples were collected during admission and postoperatively on a daily basis in vacuum tubes containing ethylenediaminetetraacetic acid for complete blood count measurements and analyzed. Complete blood count, including white blood cell count, hemoglobin level, and platelet count, was analyzed using an automated hematology analyzer.
Preoperative nutritional status was assessed using the PNI, calculated by the following formula:
PNI = (10 × serum albumin) + (0.005 × total lymphocyte count).21
Data Analysis
Continuous variables were summarized as means and SDs, while categorical variables were summarized as frequencies and percentages. Student’s
To minimize bias, PSM was applied, matching patients in a 1:4 ratio based on age, sex, EF, and comorbidities. The nearest neighbor method without replacement and a caliper of 0.2 were used.
A multiple logistic regression model was constructed to identify predictors of mortality. Variables for inclusion in the model were selected based on clinical relevance and statistical significance in univariate analysis (
A statistical significance level of
Results
A total of 440 patients were included in the study. The basic characteristics and clinical data are presented in
According to
The study population comprised 440 patients undergoing open-heart surgery, with a mean age of 65.2 years (range: 27-84 years). Among the patients, 68.64% were male, and 31.36% were female. The prevalence of DM was 58.18%, while HT was present in 37.5% of patients. The overall mortality rate (MR) in this cohort was 21.82% (MR = 21.82%,
The mean EF of the patients was 51.1% (range: 30%-64%). Preoperative biochemical parameters showed a mean creatinine level of 0.81 mg/dL and a median of 0.91 mg/dL (range: 0.45-9.50 mg/dL). The mean preoperative urea level was 39.1 mg/dL (range: 17.0-113.5 mg/dL). The neutrophil count varied from 1.02 to 15.5 × 10³/µL, with a mean of 5.6 × 10³/µL, while the lymphocyte count had a mean of 2.05 × 10³/µL, ranging from 0.35 to 5.80 × 10³/µL.
The preoperative PNI showed a mean value of 86.31 and a median of 84.99 (range: 9.33-203.52). C-reactive protein levels varied significantly, with a mean of 24.1 mg/L (range: 0.45-410.32 mg/L). Serum albumin levels had a mean of 36.87 mg/L (range: 25.0-47.1 mg/L).
Surgical parameters revealed that the mean cardiopulmonary bypass (CPB) duration was 118.8 minutes (range: 37-250 minutes), while the mean cross-clamp duration was 71.3 minutes (range: 13-140 minutes).
The patient population was predominantly male, with a high prevalence of diabetes and hypertension. Wide variability in biochemical markers highlights the heterogeneity of the cohort. The broad range of PNI values underscores its relevance in risk assessment. Differences in CPB and cross-clamp durations reflect variations in surgical complexity.
According to
Patients who did not survive had significantly lower EF (49.8 ± 9.5 vs. 52.3 ± 6.9,
Both preoperative and postoperative PNI values were significantly lower in deceased patients [Pre-PNI: 43.23 ± 26.71 vs. 73.67 ± 29.64, (OR = 0.95,
Diabetes mellitus was significantly more prevalent among survivors [81.25% vs. 18.75%, (OR = 3.12,
Lower EF, higher postoperative creatinine and urea levels, and reduced postoperative PNI were strongly associated with mortality. The significant decline in postoperative albumin and elevated inflammatory markers suggest a higher burden of systemic stress in non-survivors. Diabetes showed a notable relationship with survival, indicating a potential protective factor in this cohort.
According to
Logistic regression analysis revealed that EF was significantly associated with mortality, with each 1-unit increase reducing the risk of death by 9% (OR = 0.91,
Diabetes mellitus was strongly associated with increased mortality risk, with diabetic patients having a 3.12 times greater risk of death (OR = 3.12,
Lower ejection fraction and diabetes mellitus significantly increased mortality risk. Male patients had a higher likelihood of death, emphasizing a potential gender-related impact. Hypertension and age were not significant predictors of mortality in this cohort. These findings highlight the importance of cardiac function and metabolic health in perioperative risk stratification.
According to
Logistic regression analysis demonstrated a significant association between preoperative urea levels and mortality, with each 1 mg/dL increase raising the risk of death by 5% (OR = 1.05,
Preoperative albumin levels also showed a significant inverse relationship with mortality, with each 1 mg/L increase lowering the risk of death by 19% (OR = 0.81,
Low preoperative PNI and albumin levels were strong predictors of mortality, emphasizing the importance of nutritional status in surgical outcomes. Elevated preoperative urea levels also increased mortality risk, reflecting potential metabolic stress. Other biochemical markers, including creatinine and inflammatory parameters, did not show a significant impact on mortality.
According to
Logistic regression analysis revealed that postoperative creatinine was a strong predictor of mortality, with each 1 mg/dL increase associated with a 2.85-fold higher risk of death (OR = 2.85,
Postoperative PNI showed a strong protective effect, where each 1-unit increase reduced mortality risk by 6% (OR = 0.94,
Among inflammatory markers, postoperative neutrophils and postoperative lymphocytes were significantly associated with mortality, with each 1-unit increase raising the risk by 22% (OR = 1.22,
Elevated postoperative creatinine, urea, and inflammatory markers were significantly linked to increased mortality, reflecting the critical role of kidney function and systemic response in surgical outcomes. Low postoperative PNI and albumin levels were strong predictors of poor prognosis, emphasizing the need for nutritional optimization. Postoperative platelet levels appeared to have a protective effect, while CRP did not show a significant impact.
Discussion
This single-center retrospective study demonstrates that both preoperative and postoperative PNI values are strong predictors of mortality following CABG. The robust association between PNI and surgical outcomes strongly advocates for routine, comprehensive nutritional assessments as part of preoperative care in cardiac surgery.
Several tools are utilized to assess nutritional status prior to surgery. Tools like the Malnutrition Universal Screening Tool, Mini Nutritional Assessment, and Short Nutritional Assessment Questionnaire have been identified as independent predictors of postoperative complications in cardiac surgery.23,
The concept of the PNI was introduced by Budczies and colleagues in 1980.28 Onodera and colleagues subsequently modified the original PNI equation to incorporate serum albumin levels and peripheral lymphocyte counts.29 Prognostic Nutritional Index is calculated based on serum albumin concentration and peripheral blood lymphocyte count, making it a reliable indicator of disease severity in patients undergoing heart surgery. Recent studies related to cardiovascular diseases have reported that lower PNI values are significantly associated with higher mortality rates.30-
Prognostic Nutritional Index is particularly advantageous because it is a simple, cost-effective measure that does not require specialized equipment, making it easy to implement in clinical practice. Implementing routine nutritional screening could lead to improved risk stratification and patient outcomes in cardiac surgery. However, the impact of PNI on cardiac surgery outcomes has not been extensively studied. Future research should also focus on assessing PNI in diverse populations, as variations in comorbidities may influence its predictive value. Keskin et al34 reported a significant correlation between PNI score and both in-hospital and long-term mortality in CABG patients. These findings are consistent with Keskin et al34, as the authors also observed a strong association between lower PNI and increased mortality in CABG patients, both preoperatively and postoperatively, underscoring its predictive value. Postoperative PNI was found to be a stronger predictor of mortality than preoperative PNI. This may be due to the dynamic changes in systemic inflammation and metabolic stress occurring during the early postoperative period, leading to a more accurate reflection of physiological resilience. As an additional finding in the study, CRP did not demonstrate a statistically significant association with postoperative mortality. This may be due to its variability in response to perioperative factors such as surgical stress, transient inflammatory reactions, and secondary complications, which may limit its prognostic value in CABG patients. Hayashi et al35 found that higher PNI scores were associated with shorter mechanical ventilation times, shorter intensive care unit (ICU) stays, and lower infection rates.35 Similarly, this study revealed that postoperative PNI scores were significant predictors of early mortality, further supporting Hayashi et al’s findings that improved nutritional status can positively influence postoperative outcomes. They noted that in multivariate analyses, low PNI scores were among the independent predictors of mortality. Lee et al36 evaluated the use of PNI scores in adult patients undergoing their first heart surgery and found that lower PNI predicted early mortality and morbidity independently and was associated with longer mechanical ventilation and ICU stay. These results align with those of Lee et al,36 as the authors demonstrated that both preoperative and postoperative PNI scores were independent predictors of early mortality, reinforcing the role of PNI in risk stratification for CABG patients. In a previous study on patients with acute heart failure, it was shown that PNI was independently associated with long-term survival.37 While prior studies have focused on long-term survival in heart failure patients, this study uniquely demonstrates the impact of PNI on short-term mortality in CABG patients, emphasizing its utility in both pre- and postoperative settings.
The authors suggested that PNI reflects cardiac cachexia in heart failure patients and may be an independent risk factor for mortality in these patients. While Cheng et al37 highlighted PNI’s significance in heart failure patients, this study extends this observation to CABG patients, where lower PNI scores were closely linked to higher mortality, particularly in the postoperative phase. A multidisciplinary approach involving dietitians and surgeons can optimize preoperative care and enhance patient outcomes.
Previous studies have examined the relationships between preoperative PNI measurements and mortality and morbidity. However, no studies have investigated the impact of both preoperative and postoperative PNI measurements on mortality. This study explores this relationship, particularly finding that postoperative PNI is a good early indicator of mortality. Ultimately, the integration of PNI into clinical practice could refine surgical risk assessments and enhance patient management strategies.
Study Limitations
This study has several limitations. While a relatively large patient cohort was analyzed, the single-center, retrospective design limited the ability to conduct subgroup analyses for high-risk patients, such as those with heart failure or undergoing emergency surgery. Additionally, the underlying pathophysiology linking PNI with early complications in cardiac surgery remains unclear. Despite efforts to minimize bias by focusing on CABG patients and using multivariate analysis, unmeasured variables may have influenced the results. The study was further limited by assessing only all-cause mortality without analyzing specific causes of death. Larger, randomized trials are needed to validate PNI’s utility and its impact on clinical outcomes.
Conclusions
Prognostic Nutritional Index proves to be a robust and reliable predictor of mortality in CABG patients, emphasizing its value in enhancing both preoperative and postoperative risk assessments. The strong association between lower PNI values—particularly postoperative reductions—and increased mortality emphasizes the critical role of this index in identifying high-risk patients. Prognostic Nutritional Index should be integrated into routine preoperative and postoperative risk stratification protocols to optimize surgical outcomes. Integrating PNI into routine surgical protocols could significantly enhance mortality risk stratification, enabling timely and targeted interventions. Future large-scale studies are essential to validate its prognostic accuracy and further define its role in improving surgical outcomes through precise mortality prediction.
Footnotes
References
- Ralapanawa U, Sivakanesan R. Epidemiology and the magnitude of coronary artery disease and acute coronary syndrome: a narrative review. J Epidemiol Glob Health. 2021;11(2):169-177.
- Székely A, Nussmeier NA, Miao Y. A multinational study of the influence of health-related quality of life on in-hospital outcome after coronary artery bypass graft surgery. Am Heart J. 2011;161(6):1179-1185.e2.
- Thuijs DJFM, Kappetein AP, Serruys PW. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomised controlled SYNTAX trial. Lancet. 2019;394(10206):1325-1334.
- Glance LG, Lustik SJ, Hannan EL. The Surgical Mortality Probability Model: derivation and validation of a simple risk prediction rule for noncardiac surgery. Ann Surg. 2012;255(4):696-702.
- Hardiman SC, Villan Villan YF, Conway JM, Sheehan KJ, Sobolev B. Factors affecting mortality after coronary bypass surgery: a scoping review. J Cardiothorac Surg. 2022;17(1):-.
- Zhao Y, Yu X, Ma X, Zhang L, Wang Z. Outcomes and risk factors associated with in-hospital mortality in patients undergoing coronary artery bypass grafting with low ejection fraction. Front Cardiovasc Med. 2024;11():-.
- Ohri SK, Benedetto U, Luthra S. Coronary artery bypass surgery in the UK, trends in activity and outcomes from a 15-year complete national series. Eur J Cardiothorac Surg. 2022;61(2):449-456.
- Hannan EL, Zhong Y, Lahey SJ. 30-day readmissions after coronary artery bypass graft surgery in New York State. JACC Cardiovasc Interv. 2011;4(5):569-576.
- Habib RH, Dimitrova KR, Badour SA. CABG versus Primate Conservation: greater benefit in long-term outcomes with multiple arterial bypass grafting. J Am Coll Cardiol. 2015;66(13):1417-1427.
- Reames BN, Ghaferi AA, Birkmeyer JD, Dimick JB. Hospital volume and operative mortality in the modern era. Ann Surg. 2014;260(2):244-251.
- Mejia OAV, Lisboa LAF, Caneo LF. Analysis of> 100,000 cardiovascular surgeries performed at the heart institute and a new era of outcomes. Arq Bras Cardiol. 2020;114(4):603-612.
- Fortescue EB, Kahn K, Bates DW. Development and validation of a clinical prediction rule for major adverse outcomes in coronary bypass grafting. Am J Cardiol. 2001;88(11):1251-1258.
- Padmanabhan H, Siau K, Curtis J. Preoperative anemia and outcomes in cardiovascular surgery: systematic review and meta-analysis. Ann Thorac Surg. 2019;108(6):1840-1848.
- Cooper WA, O’Brien SM, Thourani VH. Impact of renal dysfunction on outcomes of coronary artery bypass surgery: results from the Society of Thoracic Surgeons National Adult Cardiac Database. Circulation. 2006;113(8):1063-1070.
- Bukkapatnam RN, Yeo KK, Li Z, Amsterdam EA. Operative mortality in women and men undergoing coronary artery bypass grafting (from the California Coronary Artery Bypass Grafting Outcomes Reporting Program). Am J Cardiol. 2010;105(3):339-342.
- Chen-Scarabelli C. . Female Gender Is Not Predictive of Hospital Mortality After Coronary Artery Bypass Graft Surgery. 2010;():A193-A193.
- Koch CG, Li L, Kaplan GA. Socioeconomic position, not race, is linked to death after cardiac surgery. Circ Cardiovasc Qual Outcomes. 2010;3(3):267-276.
- Shahian DM, O’Brien SM, Sheng S. Predictors of long-term survival after coronary artery bypass grafting surgery: results from the Society of Thoracic Surgeons Adult Cardiac Surgery Database (the ASCERT study). Circulation. 2012;125(12):1491-1500.
- Nashef SA, Roques F, Michel P, Gauducheau E, Lemeshow S, Salamon R. European system for cardiac operative risk evaluation (EuroSCORE). Eur J Cardiothorac Surg. 1999;16(1):9-13.
- Kurumisawa S, Kawahito K. Risk analysis using the prognostic nutritional index in hemodialysis-dependent patients undergoing cardiac surgery. J Artif Organs. 2018;21(4):443-449.
- Tokunaga R, Sakamoto Y, Nakagawa S. Prognostic nutritional index predicts severe complications, recurrence, and poor prognosis in patients with colorectal cancer undergoing primary tumor resection. Dis Colon Rectum. 2015;58(11):1048-1057.
- Norman G. Likert scales, levels of measurement, and the “laws” of statistics. Adv Health Sci Educ Theory Pract. 2010;15(5):625-632.
- Lomivorotov VV, Efremov SM, Boboshko VA. Evaluation of nutritional screening tools for patients scheduled for cardiac surgery. Nutrition. 2013;29(2):436-442.
- Lomivorotov VV, Efremov SM, Boboshko VA. Prognostic value of nutritional screening tools for patients scheduled for cardiac surgery. Interact Cardiovasc Thorac Surg. 2013;16(5):612-618.
- Stoppe C, Goetzenich A, Whitman G. Role of nutrition support in adult cardiac surgery: a consensus statement from an International Multidisciplinary Expert Group on Nutrition in Cardiac Surgery. Crit Care. 2017;21(1):1-.
- Morgan TM, Tang D, Stratton KL. Preoperative nutritional status is an important predictor of survival in patients undergoing surgery for renal cell carcinoma. Eur Urol. 2011;59(6):923-928.
- Yeh DD, Fuentes E, Quraishi SA. Adequate nutrition may get you home: effect of caloric/protein deficits on the discharge destination of critically ill surgical patients. JPEN J Parenter Enter Nutr. 2016;40(1):37-44.
- Budczies J, Klauschen F, Sinn BV. Cutoff Finder: a comprehensive and straightforward Web application enabling rapid biomarker cutoff optimization. PLoS One. 2012;7(12):-.
- Kanda M, Mizuno A, Tanaka C. Nutritional predictors for postoperative short-term and long-term outcomes of patients with gastric cancer. Medicine. 2016;95(24):-.
- Basta G, Chatzianagnostou K, Paradossi U. The prognostic impact of objective nutritional indices in elderly patients with ST-elevation myocardial infarction undergoing primary coronary intervention. Int J Cardiol. 2016;221():987-992.
- Keskin M, Hayıroğlu MI, Keskin T. A novel and useful predictive indicator of prognosis in ST-segment elevation myocardial infarction: the prognostic nutritional index. Nutr Metab Cardiovasc Dis. 2017;27(5):438-446.
- Hayıroğlu Mİ, Keskin M, Keskin T. A novel independent survival predictor in pulmonary embolism: prognostic nutritional index. Clin Appl Thromb Hemost. 2018;24(4):633-639.
- Ozluk OA, Arican Ozluk O, Yildirim Turan E. Immune system’s status affects the infective endocarditis hospital mortality. Int J Immunol. 2020;8(1):9-12.
- Keskin M, İpek G, Aldağ M. Effect of nutritional status on mortality in patients undergoing coronary artery bypass grafting. Nutrition. 2018;48():82-86.
- Hayashi J, Uchida T, Ri S. Clinical significance of the prognostic nutritional index in patients undergoing cardiovascular surgery. Gen Thorac Cardiovasc Surg. 2020;68(8):774-779.
- Lee SI, Ko KP, Choi CH, Park CH, Park KY, Son KH. Does the prognostic nutritional index have a predictive role in the outcomes of adult cardiac surgery?. J Thorac Cardiovasc Surg. 2020;160(1):145-153.e3.
- Cheng YL, Sung SH, Cheng HM. Prognostic nutritional index and the risk of mortality in patients with acute heart failure. J Am Heart Assoc. 2017;6(6):-.


