2Department of Public Health, Faculty of Medicine, Adıyaman University, Adıyaman, Türkiye
Abstract
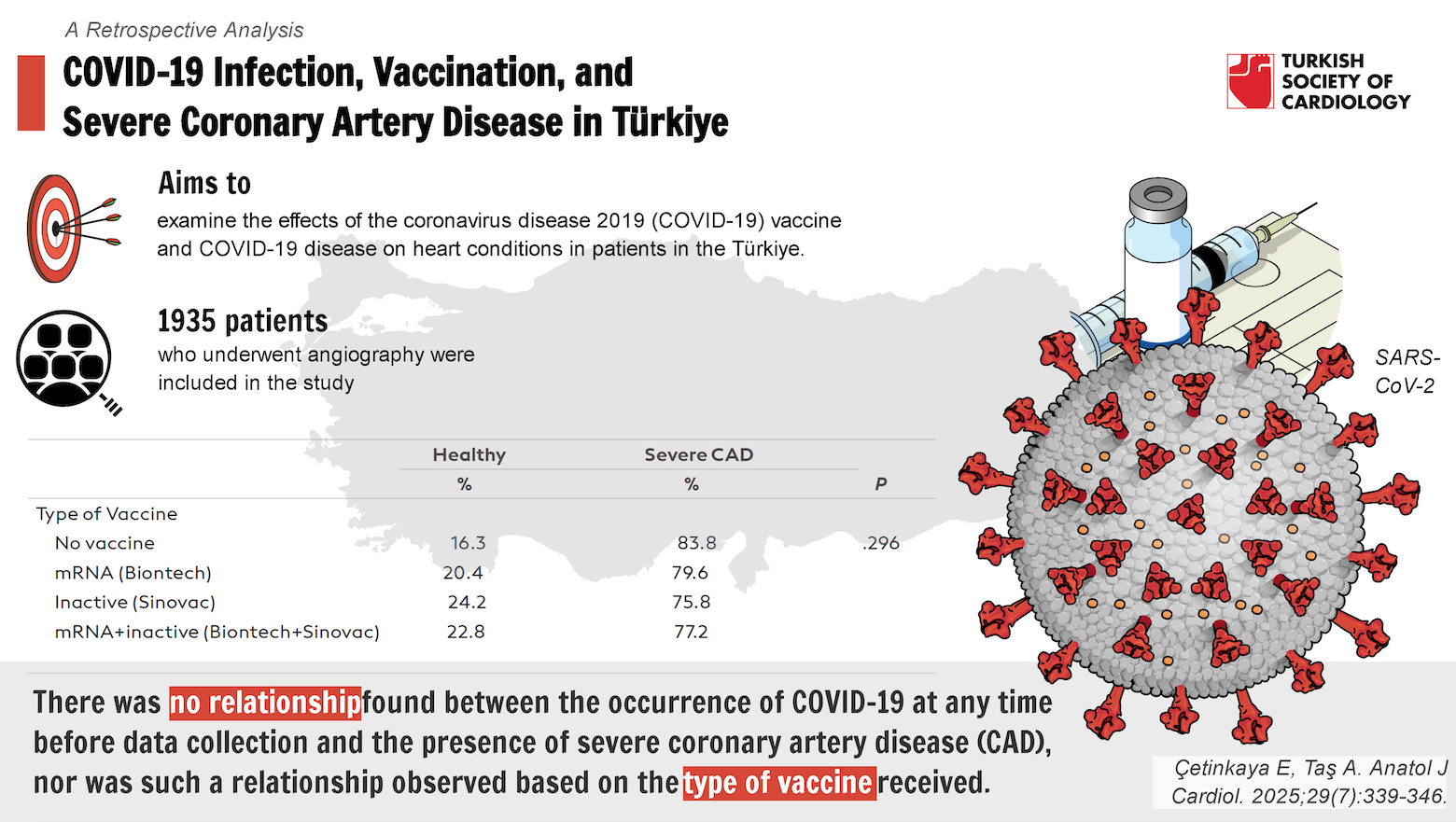
Background: This study addresses a topic that has been explored globally but has not yet been investigated in the Türkiye. Considering that all diseases and treatments may vary due to genetic diversity, the aim is to examine the effects of the coronavirus disease 2019 (COVID-19) vaccine and COVID-19 disease on heart conditions in patients in the Türkiye.
Methods: A total of 1935 patients who underwent angiography were included in the study. Descriptive statistics were provided in terms of numbers and percentages, as well as means and SD.
Results: There was no relationship found between the occurrence of COVID-19 at any time before data collection and the presence of severe coronary artery disease (CAD). Additionally, there was no relationship found between the time elapsed between COVID-19 infection and angiography and the presence of severe CAD among individuals who underwent angiography at a later date (n = 689). Between November 2021 and May 2022 (fifth 6 months) and May 2022 and November 2022 (sixth 6 months), the rates of severe CAD in angiograms conducted compared to the baseline were higher. There was no significant relationship found between the number of doses of messenger ribonucleic acid (mRNA) vaccine received and the risk of developing severe CAD (P = .139). Similarly, there was no significant relationship found between the number of doses of inactivated vaccine received and the risk of developing severe CAD (P = .382).
Conclusion: In the long term, neither infection nor vaccination increases the risk of cardiovascular disease, regardless of the time elapsed since the COVID-19 infection or the type of vaccination received.
Graphical Abstract
Hıghlıghts
- There was no significant relationship between having a COVID-19 infection and the presence of severe CAD, even when analyzed over time after infection (39).
- Neither receiving mRNA vaccines nor inactivated vaccines showed a significant association with the risk of severe CAD, regardless of the number of doses or time elapsed since vaccination (05).
- A notable increase in the rate of severe CAD was observed in angiograms conducted during the fifth (November 2021-May 2022) and sixth (May 2022-November 2022) 6-month periods compared to baseline (001).
- Individuals vaccinated with mRNA vaccines had a significantly lower rate of COVID-19 infection compared to unvaccinated individuals and those receiving inactivated vaccines (001).
- Although not statistically significant, patients who received at least 1 dose or 2 or more doses of the vaccine showed lower rates of severe CAD at 1-3 months, 3-6 months, and 18-36 months post-vaccination compared to unvaccinated groups.
Introductıon
Coronavirus disease 2019 (COVID-19), exhibiting global spread, has become one of the deadliest diseases of the twenty-first century. The disease has been observed in 774 954 393 individuals and has caused 7 040 264 deaths from December 2019 to March 2024.1 The disease that began in December 2019 in the city of Wuhan, China, clinically manifests itself with symptoms such as fever, cough, difficulty breathing, and joint and muscle pain.2
Long-term effects of the disease may include parenchymal damage caused by the virus in the lungs and respiratory system-related symptoms such as dyspnea, hypoxia, and pulmonary fibrosis; thromboembolisms due to microvascular damage associated with immune response; and cardiac effects resulting from myocardial and microvascular damage including chest pain, pericarditis, myocarditis, fibrosis, arrhythmias, and cardiac death. Additionally, various systemic symptoms such as neuropsychiatric and cognitive dysfunction, hair loss, urticarial lesions, appetite loss, diarrhea, new-onset diabetes, subacute thyroiditis, glomerular, and tubular diseases can occur.3
Reviews have shown that COVID-19 disease can lead to acute myocardial infarction, myocarditis, heart failure, Takotsubo syndrome, venous thromboembolic events, and arrhythmias in both the short and long term on the cardiac system.3,
During the COVID-19 pandemic, studies have shown not only the long-term cardiac side effects of the virus but also an increase in mortality rates compared to pre-pandemic levels. This rise is attributed to delays in hospital visits and the presence of COVID-19 infections in patients admitted with other diagnoses. In the early phase of the pandemic, certain centers observed that both percutaneous interventions and open-heart surgeries were performed under more urgent conditions, while elective cases were postponed.10-
In the study region, in recent years, there has been an increase in the daily case numbers compared to previous years, as well as an increase in the number of patients with significant coronary artery disease (CAD) in coronary angiography among these cases. It is believed that this increase in the number of cases with severe CAD may be associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection or the vaccination program. To investigate the relationship between the increase in cases with severe CAD and SARS-CoV-2 infection or vaccination, the patients presented to the center were reviewed retrospectively. Being the sole primary center in the study region for patients experiencing heart attacks in this region has allowed the authors to demonstrate any increase in cases compared to the pre-pandemic period.
The aim of this study was to address the low health literacy in the region and counteract widespread vaccine hesitancy, which is prevalent both regionally and nationally. Many attribute various heart diseases to vaccinations, impacting public trust in hospital-recommended treatments, including vaccinations. This study also aims to strengthen the credibility of hospital-provided guidance and recommendations. Furthermore, it seeks to provide scientific clarity on the misconception, present even among some healthcare professionals, that vaccinations have led to an increase in ACS and other severe CADs.
Methods
This retrospective cross-sectional study involved accessing the medical records of patients who underwent angiography at the study hospital between November 2019 and October 2023. Data for the study were collected and evaluated between November 2023 and January 2024. The study was initiated with the approval of the Ethics Committee on April 28, 2023, under protocol number E-95531838-050.99-83973. A total of 1935 patients who underwent angiography at the authors’ cardiology clinic between November 2019 and October 2023 were included in the study. Due to only being able to access vaccination data for living patients, vaccination-related analyses were conducted on 1629 patients and comprising 1598 patients who underwent percutaneous coronary intervention for significant CAD as determined through coronary angiography, and 339 patients for whom an operation decision was made. Both of them accepted as having severe CAD. Coronary angiographies of patients were performed and evaluated by expert interventional cardiologists working at the study hospital using Siemens Heathcare GmbH, Henkestr, 127 91052 Erlangen, Germany, Model 10562561, devices available at the study hospital, both during regular working hours and on-call duties.
Initially, all the reports of patients with significant CAD who had undergone coronary angiography were accessed through the KARMED hospital database. Health Information Management System (HSYS) is a nationwide online public health management data system under the Turkish Ministry of Health, allowing for the retrieval of COVID infection data using patients’ national identification numbers. Health Information Management System is a centralized healthcare management system in Türkiye, used for collecting, managing, and analyzing patient data across healthcare facilities to improve the efficiency and coordination of healthcare services. During the COVID-19 pandemic period, with the modules defined in the HSYS system, the evaluation of polymerase chain reaction test results of COVID-19 patients by healthcare personnel performing filiation, tracing of contacts, and follow-up of patients and contacts were carried out through the HSYS system. Similarly, AŞILA is an official platform, similar to HSYS, that records vaccination data and was accessed using patients’ national identification numbers from the onset of the pandemic. AŞILA (Vaccination Information Management System) is a national system for managing vaccination records, enabling real-time tracking of vaccination status, doses, and distribution throughout Türkiye, particularly useful for monitoring COVID-19 vaccination coverage and schedules. By entering the ID numbers of individuals into the system, the barcode of their COVID-19 vaccines is scanned through the camera of the mobile application and the vaccine to be administered is recorded in the system. The system is designed to view individuals’ vaccination statuses and facilitate vaccine administration; therefore, the vaccination statuses of deceased individuals cannot be evaluated through the AŞILA application.
Data on patient age, gender, COVID-19 infection history, the timing of infection, and vaccination records, including the number of doses administered and the specific vaccine used, were analyzed using data from KARMED, HSYS, and AŞILA systems. A monthly analysis revealed an increase in the number of patients visiting the study center after the pandemic. The study identified the number of patients who were vaccinated, unvaccinated, or had previously contracted the infection, as well as the time interval between infection and the procedure for significant CAD. By comparing the findings with existing literature, the research aimed to determine whether COVID-19 infection had contributed to an increase in the incidence of significant CAD in the study region.
The study was conducted in accordance with the principles of the Declaration of Helsinki. No artificial intelligence (AI)-assisted technologies, such as Large Language Models, chatbots, or image creators, were used in the production of this submitted work. All content was created entirely by the authors without the aid of AI tools.
Statistical Analysis
The data obtained from the study were analyzed using the Statistical Package for the Social Sciences (SPSS) version 19.0 software (IBM Corp., Armonk, NY, USA). The Kolmogorov-Smirnov test was conducted to assess the normality of distribution. Descriptive statistics were presented as frequency and percentage [n (%)] for categorical variables, and as median with interquartile range (25th-75th percentile) for continuous variables that did not follow a normal distribution. All of the continious data did not follow a normal distribution, Mann–Whitney U-test was used for the comparison of continuous measurements between the 2 independent groups. The chi-square test was utilized to assess the relationship between categorical variables. Bonferroni correction was used for post hoc analysis.
Results
The study included 71.9% male participants out of 1935 individuals. The median age was 64.00 (57.00-73.00). About 79.4% of the participants who underwent angiography were diagnosed with severe CAD. At the time of data collection, 15.8% of the patients were deceased (
Starting from 3 months prior to the date of the first COVID-19 case, patients were evaluated in 6-month intervals. The first case in Türkiye was reported in February 2020, and during the period between November 2019 and May 2020, the rate of cases showing as healthy in angiographies was high. However, in the second, third, and fourth 6-month periods, no difference was observed between angiogram results showing severe CAD and being healthy. On the other hand, between November 2021 and May 2022 (fifth 6-month interval) and May 2022 and November 2022 (sixth 6-month interval), the rates of severe CAD in angiograms conducted compared to the baseline were higher (
Due to the nature of the data collection system, vaccination data could not be obtained for 306 individuals who had previously died. Among the individuals for whom vaccination data were available (n = 1629), 4.2% had not received any vaccine, while 90.6% had received at least 2 doses of vaccine. Among the participants who were alive, 56.8% had received at least 2 doses of mRNA vaccine, and 39.9% had received at least 2 doses of inactivated vaccine. The median total number of vaccine doses received by vaccinated individuals was 2.00 (2.00-3.00), with an median of 2.00 (1.00-2.00) doses of mRNA vaccine and 0.00 (0.00-2.00) doses of inactivated vaccine. There was no significant relationship found between the number of doses of mRNA vaccine received and the risk of developing severe CAD (
A detailed statistical analysis was conducted to examine whether there is a relationship between the frequency and timing of vaccination and the diagnosis of severe CAD, as well as any association between the time elapsed since a COVID-19 infection and the risk of severe CAD diagnosis. This analysis was performed across relevant time intervals to ensure clarity. No relationship was found when comparing individuals who had never been vaccinated and those who had received at least 1 dose of vaccination, as well as healthy individuals and those diagnosed with CAD, across 1-, 3-, 6-, 9-, 12-, 18-, and 36-month intervals following vaccination (
The relationship between vaccination status and CAD was assessed by grouping individuals with a CAD diagnosis and healthy individuals into categories of those who had never been vaccinated and those who had received at least 1 dose, as well as those who had received fewer than 2 doses and those who had received 2 or more doses. Patients who received at least 1 dose of the vaccine, rate of severe CAD after 1-3 months, 3-6 months, and 18-36 months post-first dose was lower compared to those who were unvaccinated. Similarly, in individuals who received 2 or more doses, rate of severe CAD was lower compared to those who received fewer than 2 doses. However, this reduction was not statistically significant (
Patients who underwent angiography due to complaints of chest pain were grouped according to the time elapsed between COVID-19 infection and angiography. Accordingly, no relationship was found between duration after COVID-19 infection and diagnosis of severe CAD. There was no relationship found between the time elapsed after the first dose of vaccine and the development of severe CAD in vaccinated patients. (
When patients were grouped according to the types of vaccines they received, it was observed that individuals who received mRNA vaccines had lower rates of COVID-19 compared to those who were unvaccinated and those who received inactive vaccines (
Discussion
In this study, angiographies conducted in 6-month intervals were followed in the post-COVID-19 period. It was found that there was an increase in the frequency of severe CAD diagnosis in angiographies conducted in the fifth and sixth 6-month intervals after the COVID-19 pandemic. Studies were conducted in the United States, Austria, Italy, and Spain, Türkiye have shown a decrease in hospital admissions due to ACS during the COVID-19 period.10,
A meta-analysis has shown that the risk of developing ACS is 1.93 times higher in individuals who have had COVID-19 infection after an average follow-up of 8.5 months.19 Acute respiratory viral infections such as the flu can trigger AMI(Acute Myocardial Infarction) and stroke. However, COVID-19 patients are 7 times more likely to have a stroke compared to flu patients, and acute myocardial infarction (AMI) and stroke risks remain elevated for a year after the infection. The excessive inflammatory response seen in severe COVID-19 cases, also known as cytokine storm, may contribute to the increased risk of AMI and stroke. In the light of recent studies, it has been determined that acute cardiovascular events may occur in individuals, even those who have had SARS-CoV-2 infection without hospitalization, for up to 1 year after the infection.20 Several mechanisms have been proposed to explain cardiac damage, yet the exact pathogenic pathways remain unclear. Potential causes include cytokine-induced injury, microvascular thrombi formation, and/or direct damage to cardiomyocytes resulting from viral invasion of the myocardium. Additionally, the intense inflammatory response triggered by COVID-19 is believed to lead to catecholamine-induced microvascular dysfunction, which may contribute to COVID-19-associated Takotsubo cardiomyopathy.21 Chronic inflammation and accompanying endothelial dysfunction can increase the risk of coronary plaque instability, a proposed mechanism behind cardiovascular complications in patients with COVID-19.22 In coronary autopsy samples obtained from COVID-19 patients, infiltrating macrophages were observed to be infected by SARS-CoV-2. Lipid-laden macrophages (foam cells), a hallmark of atherosclerosis in all stages of the disease, were more susceptible to SARS-CoV-2 infection compared to other macrophages, and this susceptibility was dependent on the neuropilin-1 receptor. Severe acute respiratory syndrome coronavirus 2 induced a strong pro-atherogenic inflammatory response in both macrophages and foam cells; this response was generally recapitulated in ex vivo SARS-CoV-2 infection of human vascular tissue samples. This response may contribute to ischemic cardiovascular complications in COVID-19 patients. By the help of this results, it has been established that SARS-CoV-2 infection can induce inflammation in the coronary arteries.23,
The relationship between patients’ retrospective history of COVID-19 infection and COVID-19 vaccination status and the diagnosis of severe CAD was evaluated, but no protective or augmentative effect of having had COVID-19 or being vaccinated against severe CAD was found. It is conceivable that the increased number of severe CAD cases could be explained by the stress-induced triggering of pre-existing cardiac problems in individuals due to the psychological and economic concerns brought about by the process. Another reason could be the sedentary lifestyle and indoor air pollution associated with the curfew implemented in Türkiye, which may be related to the increasing number of severe CAD cases. However, due to the retrospective nature of the study, further research is needed to link the increased severe CAD cases to these variables.
In this study, the development of severe CAD was evaluated in 6-month intervals after vaccination, but no relationship was found between the time elapsed after the first dose of vaccines and the development of severe CAD. A cohort study has shown that especially in the elderly population, mainly ACSs development occurred after the first 24 hours following the first dose of the vaccine.25
A systematic review comparing the side effects of vaccines indicated that cardiac side effects did not occur after Sinovac vaccination, while myocarditis, pericarditis, ACS, arrhythmias, and stress cardiomyopathy were reported as side effects after BioNTech vaccination.26 There are case reports demonstrating the development of ACS following both BioNTech and Sinovac vaccinations.27,
However, in this study, separate analyses conducted based on the type of vaccine received by individuals showed no difference in the development of severe CAD compared to those who did not receive vaccination. At the same time, there was no relationship between the number of vaccine doses administered and the development of severe CAD. Although cardiac side effects have been demonstrated in various case studies following vaccinations, this study did not find a relationship between them. Considering the high morbidity and mortality of COVID-19 disease, supporting vaccination practices would be appropriate to reduce vaccine hesitancy.
According to the results of a recent large-scale cohort study conducted in Europe, COVID-19 vaccination has been shown to reduce the risk of cardiac and thromboembolic outcomes following COVID-19. These effects are particularly pronounced for acute COVID-19 outcomes and are consistent with known reductions in disease severity following vaccination compared to unvaccinated SARS-CoV-2 infection. These findings underscore the clinically significant protective effects of COVID-19 vaccination.29
In this study, mortality rates were found to be higher in patients diagnosed with severe CAD; however, no relationship was found between COVID-19 infection and mortality. Studies conducted in Ireland have shown an increase in mortality rates following COVID-19 infection.30 In a study comparing individuals who developed severe CAD after COVID-19 with those who developed severe CAD in the general population, the mortality rates were shown to be approximately 4 times higher in individuals who developed severe CAD after COVID-19.31
Study Limitations
An important limitation of the study is the inability to access vaccination data for deceased patients when evaluating vaccine data. Consequently, there is data loss in assessing the relationship between vaccination and severe CAD, and the evaluation could only be conducted on surviving individuals. This may have led to an overestimation or underestimation of the relationship between vaccines and severe CAD. Due to the lack of records regarding the cause and timing of death in this study, the strong association between deaths and the diagnosis of severe CAD or COVID-19 infection cannot be conclusively demonstrated.
Conclusıon
According to the data from this study, although there was a decrease in hospital admissions at the beginning of the COVID-19 pandemic, there was an increase in the diagnosis of severe CAD in angiographies performed from the 27th month of the pandemic onward. However, no relationship was found between the incidence of severe CAD cases and the history of COVID-19 infection or COVID-19 vaccination status. Given the rapid spread and high morbidity and mortality of COVID-19, both mRNA and inactivated vaccines did not show an association with severe CAD in this study. The necessity of vaccination to prevent the disease was demonstrated by the lower frequency of COVID-19 observed in individuals vaccinated with mRNA vaccines. The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
Supplementary Materials
Footnotes
References
- . WHO COVID-19. . 2024;():-. https://data.who.int/dashboards/covid19/deaths?n = c.
- Zeng J, Huang J, Pan L. How to balance acute myocardial infarction and COVID-19: the protocols from Sichuan Provincial People’s Hospital. Intensive Care Med. 2020;46(6):1111-1113.
- Joshee S, Vatti N, Chang C. Long-term effects of COVID-19. Mayo Clin Proc. 2022;97(3):579-599.
- Arévalos V, Ortega-Paz L, Rodríguez-Arias JJ. Acute and chronic effects of COVID-19 on the cardiovascular system. J Cardiovasc Dev Dis. 2021;8(10):128-.
- Rahman S, Montero MTV, Rowe K, Kirton R, Kunik F. Epidemiology, pathogenesis, clinical presentations, diagnosis and treatment of COVID-19: a review of current evidence. Expert Rev Clin Pharmacol. 2021;14(5):601-621.
- Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46(4):586-590.
- Vidula MK, Ambrose M, Glassberg H. Myocarditis and other cardiovascular complications of the mRNA-based COVID-19 vaccines. Cureus. 2021;13(6):e15576-.
- Boivin Z, Martin J. Untimely myocardial infarction or COVID-19 vaccine side effect. Cureus. 2021;13(3):e13651-.
- Mishra A, Komut O, Kumar A, Ete T, Megeji RD. Acute myocardial infarction after COVID-19 vaccination: a case report. Cureus. 2022;14(5):e25536-.
- Çetinkaya E, Kundi H, Aslan AN, Akçay M. Con. Ank Med J. 2023;23(2):210-221.
- Venckus V, Budrikis A, Kazlauskaite M. The impact of COVID-19 on adult cardiac surgery. Turk Gogus Kalp Damar Cerrahisi Derg. 2022;30(4):495-502.
- Baş T, Çevirme D, Zengin A, Baltacı H, Aksoy R, Kırali K. Cardiovascular surgery during the first wave of COVID-19 pandemic. Turk Gogus Kalp Damar Cerrahisi Derg. 2023;31(3):309-316.
- Braiteh N, Rehman WU, Alom M. Decrease in acute coronary syndrome presentations during the COVID-19 pandemic in upstate New York. Am Heart J. 2020;226():147-151.
- Garcia S, Albaghdadi MS, Meraj PM. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871-2872.
- De Filippo O, D’Ascenzo F, Angelini F. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383(1):88-89.
- Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020;41(19):1852-1853.
- Rodríguez-Leor O, Cid-Álvarez B, Ojeda S. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. Interv Cardiol. 2020;2(2):82-89.
- Cameli M, Pastore MC, Mandoli GE. COVID-19 and acute coronary syndromes: current data and future implications. Front Cardiovasc Med. 2020;7():593496-.
- Zuin M, Rigatelli G, Battisti V, Costola G, Roncon L, Bilato C. Increased risk of acute myocardial infarction after COVID-19 recovery: A systematic review and meta-analysis. Int J Cardiol. 2023;372():138-143.
- Katsoularis I, Fonseca-Rodríguez O, Farrington P, Lindmark K, Fors Connolly A-MF. Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: a self-controlled case series and matched cohort study. Lancet. 2021;398(10300):599-607.
- Giustino G, Croft LB, Oates CP. Takotsubo cardiomyopathy in COVID-19. J Am Coll Cardiol. 2020;76(5):628-629.
- Chatterjee NA, Cheng RK. Cardiovascular disease and COVID-19: implications for prevention, surveillance and treatment. Heart. 2020;106(15):1119-1121.
- Lamers MM, Haagmans BL. SARS-CoV-2 pathogenesis. Nat Rev Microbiol. 2022;20(5):270-284.
- Eberhardt N, Noval MG, Kaur R. SARS-CoV-2 infection triggers pro-atherogenic inflammatory responses in human coronary vessels. Nat Cardiovasc Res. 2023;2(10):899-916.
- Aye YN, Mai AS, Zhang A. Acute myocardial infarction and myocarditis following COVID-19 vaccination. QJM Int J Med. 2023;116(4):279-283.
- Ho JSY, Sia C-H, Ngiam JN. A review of COVID-19 vaccination and the reported cardiac manifestations. Singapore Med J. 2023;64(9):543-549.
- Xu J-Q, Lin C, Liu S-Y. BNT162b2 mRNA COVID-19 vaccine induces recurrent acute coronary syndromes in coronary artery disease patients with coronary stents: a case report. Am J Transl Med. 2022;6(4):185-190.
- Ou W, Wang B, Zhang G. Acute myocardial infarction after inactivated COVID-19 vaccination: a case report and literature review. Front Cardiovasc Med. 2023;10():1123385-.
- Mercade-Besora N, Li X, Kolde R. The role of COVID-19 vaccines in preventing post COVID-19 thromboembolic and cardiovascular complications: a multinational cohort study. medRxiv. 2023;28():23291997-.
- Cusack DA. COVID-19 pandemic: Coroner’s database of death inquiries with clinical epidemiology and total and excess mortality analyses in the District of Kildare March to June 2020. J Forensic Leg Med. 2020;76():102072-.
- Kite TA, Ludman PF, Gale CP. International prospective registry of acute coronary syndromes in patients with COVID-19. J Am Coll Cardiol. 2021;77(20):2466-2476.


